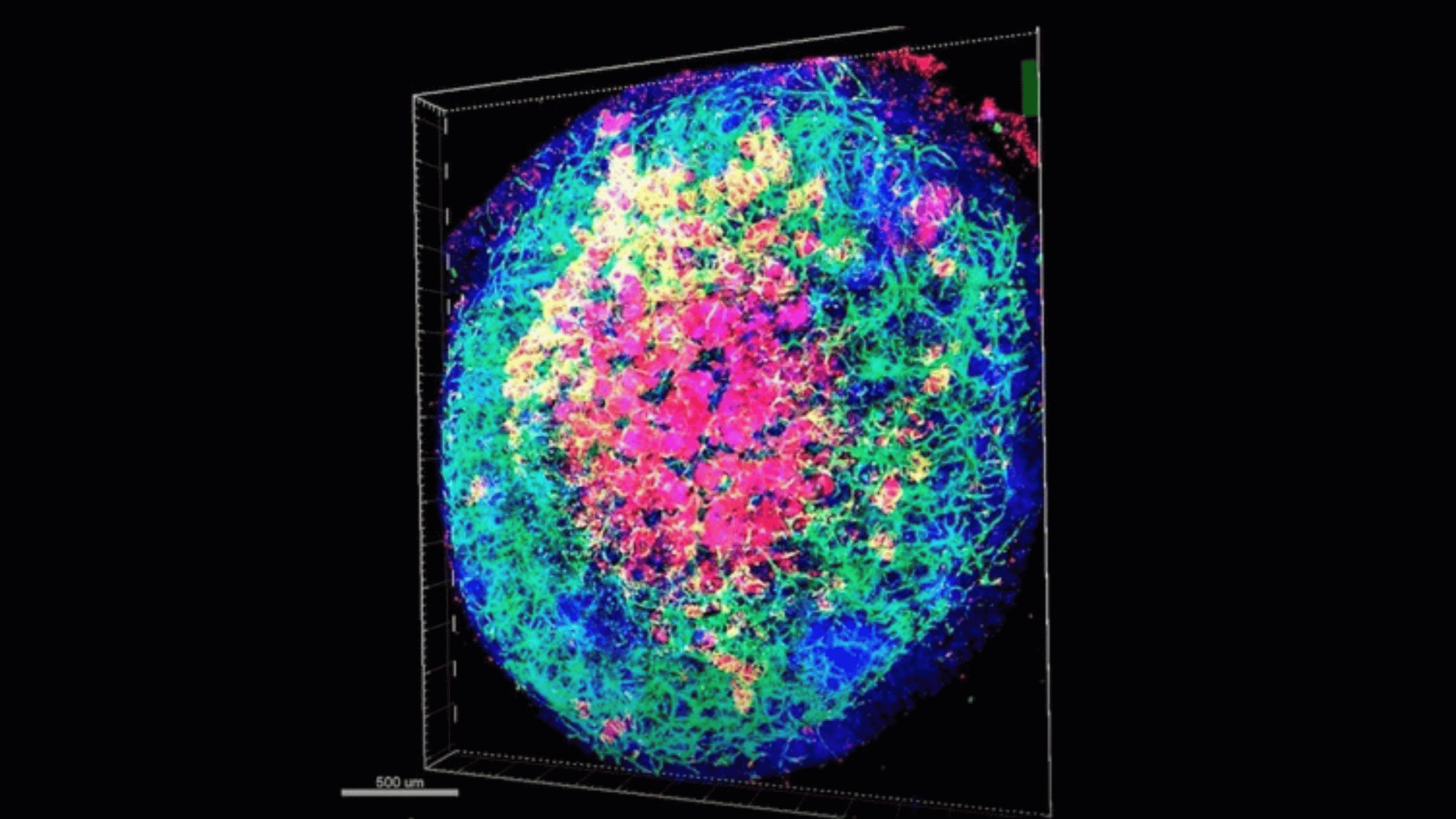
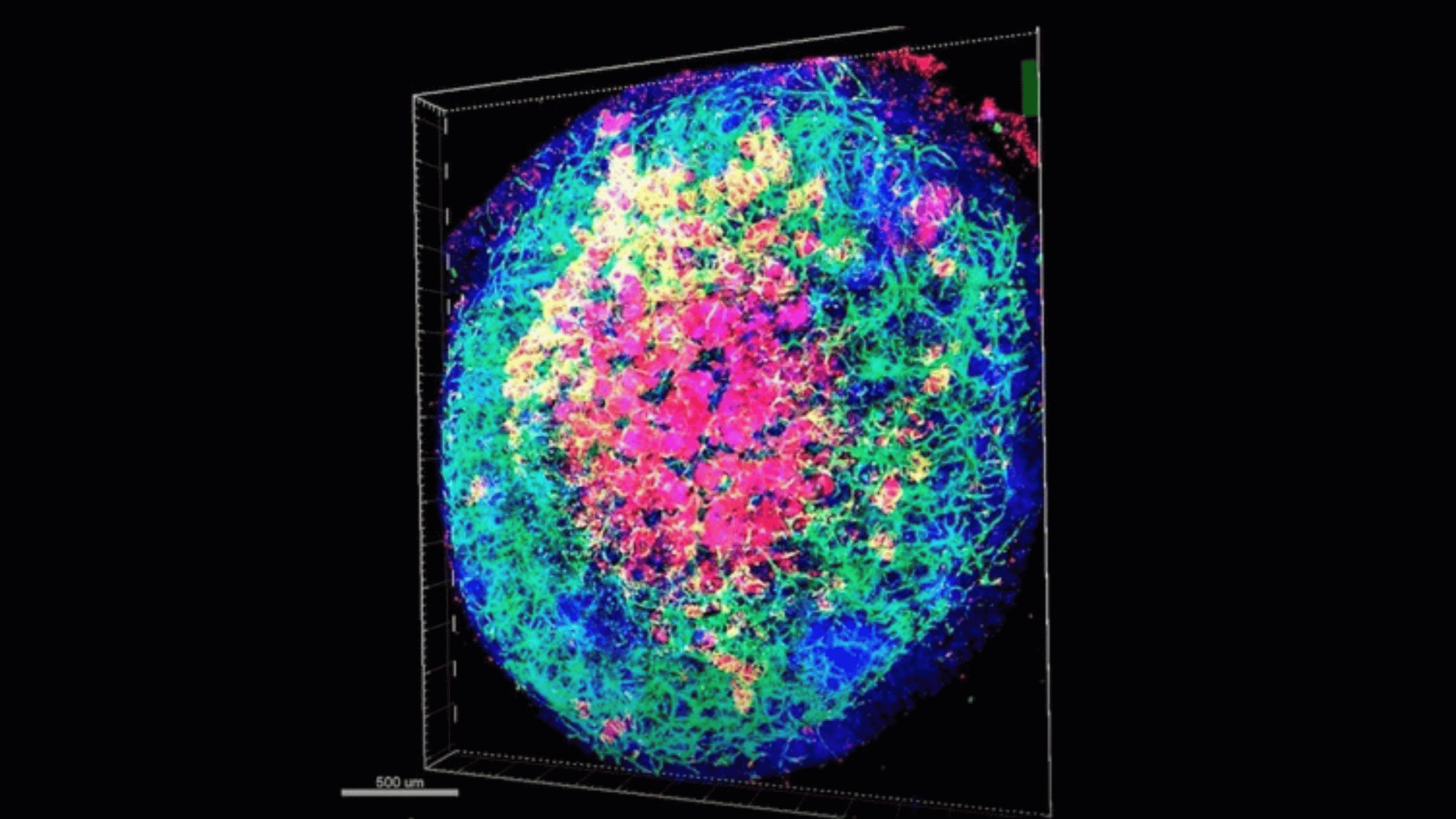
Scientists took a significant stride in regenerative medicine by successfully engineering liver tissue capable of growing internal blood vessels. Cincinnati Children’s Hospital Medical Center scientists collaborated with Japan-based colleagues to take a major leap in lab-grown organ development.
This groundbreaking development could revolutionize treatments for conditions such as hemophilia and other coagulation disorders. Additionally, it inches scientists closer to transplantable tissues for damaged livers.
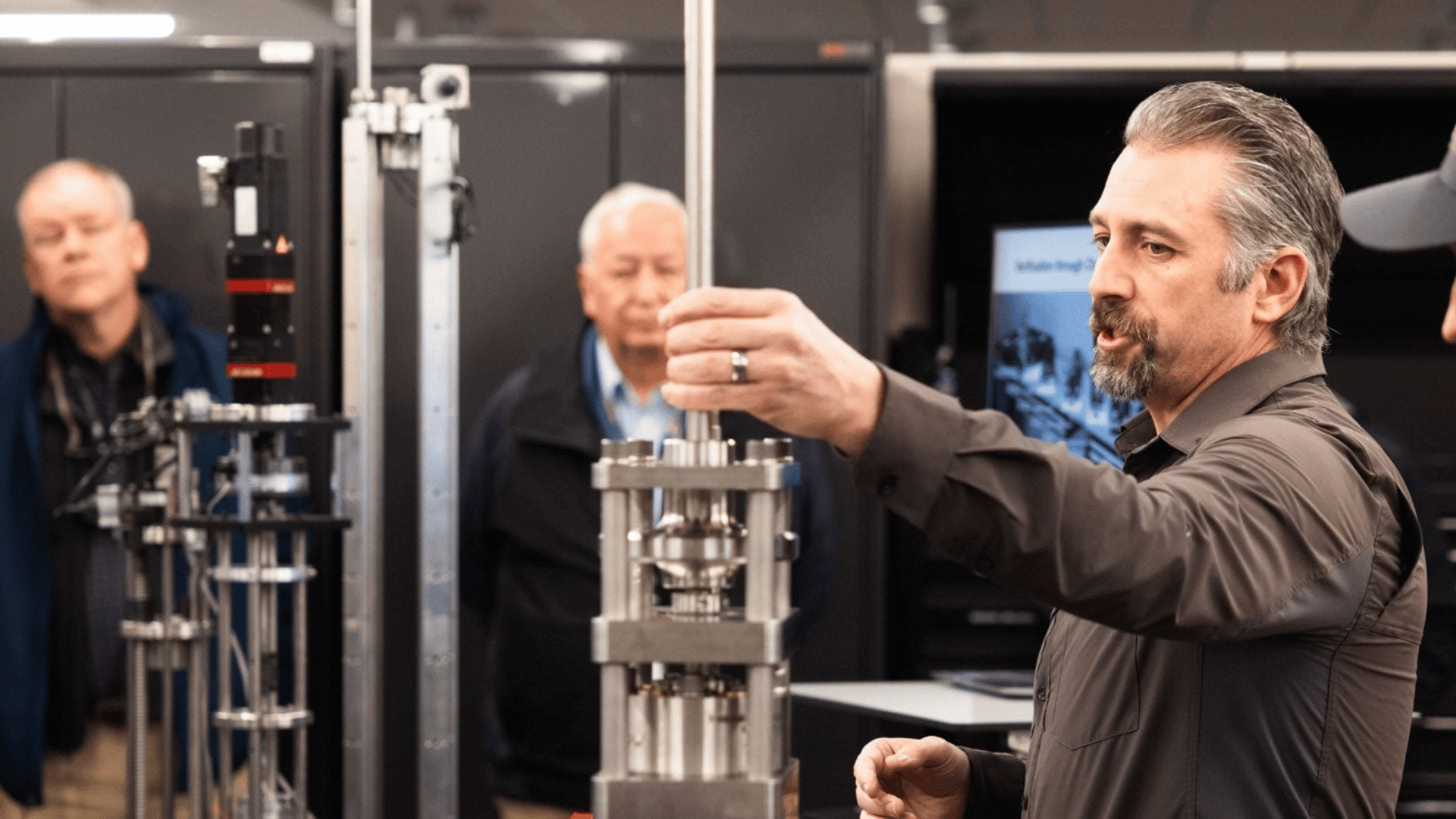
Researchers, led by Dr. Takanori Takebe, the director for commercial innovation at the Cincinnati Children’s Center for Stem Cell and Organoid Research and Medicine (CuSTOM), published their findings in Nature Biomedical Engineering.
Lab-Grown Liver
“Our research represents a significant step forward in understanding and replicating the complex cellular interactions that occur in liver development,” Dr. Takebe said. “The ability to generate functional sinusoidal vessels opens up new possibilities for modeling a wide range of human biology and disease, and treating coagulation disorders and beyond.”
Researchers around the world have tried to create miniature, lab-grown versions of organs called organoids. Scientists consider organoids as vital tools for medical research, as they hold significant promise for studying development, disease mechanisms, and drug responses.
Growing these organoids involved putting induced pluripotent stem cells (iPSCs) in specialized gels designed to turn them into specific tissue types. According to the researchers, iPSCs’ flexibility gives them a notable advantage. For example, iPSCs can be derived from generic sources or individuals with specific health conditions. Moreover, they can be gene-edited before the growing process begins.
Researchers have faced the challenge of lab-grown organoids incapable of growing essential tissues, such as nerves and blood vessels. However, the Cincinnati Children’s Hospital’s team jumped that hurdle.
Advertisement
“Ultimately, the project succeeded at differentiating human pluripotent stem cells into CD32b+ liver sinusoidal endothelial progenitors (iLSEP),” the press release states. “Then the team used an inverted multilayered air-liquid interface (IMALI) culture system to support the iLSEP cells as they self-organized into hepatic endoderm, septum mesenchyme, arterial, and sinusoidal quadruple progenitors.”
Promising Applications
Using liver-specific iLSEP progenitor cells offers a key advantage. Liver-specific progenitor cells are more likely to form vessels that function with the organoids. Positioning and timing of cell interactions were vital to a successful vessel formation.
“The success occurred in part because the different cell types were grown as neighbors that naturally communicated with each other to take their next development steps,” the study’s first author, Dr. Norikazu Saiki of the Institute of Science Tokyo, said.
There are optimistic implications for patients, including those with hemophilia, a genetic bleeding disorder. It causes repeated internal bleeding, chronic pain, and severe complications like paralysis.
“These advanced liver organoids can secrete these coagulation factors,” Dr. Takebe said. “If they can be produced at scale, they could become a viable treatment source that would benefit people who have developed inhibitors or are not indicated for gene therapy.”
It could also extend to individuals suffering from liver failure.
The press release said, “Longer-term, increasingly sophisticated liver organoids may eventually supply repair tissues that can help diseased livers heal themselves.”