Heart attacks leave behind permanent scar tissue, which forces muscles to overwork, often leading to debilitating heart failure. Researchers from Texas A&M University may offer a promising new therapeutic approach to interrupt the damaging progression.
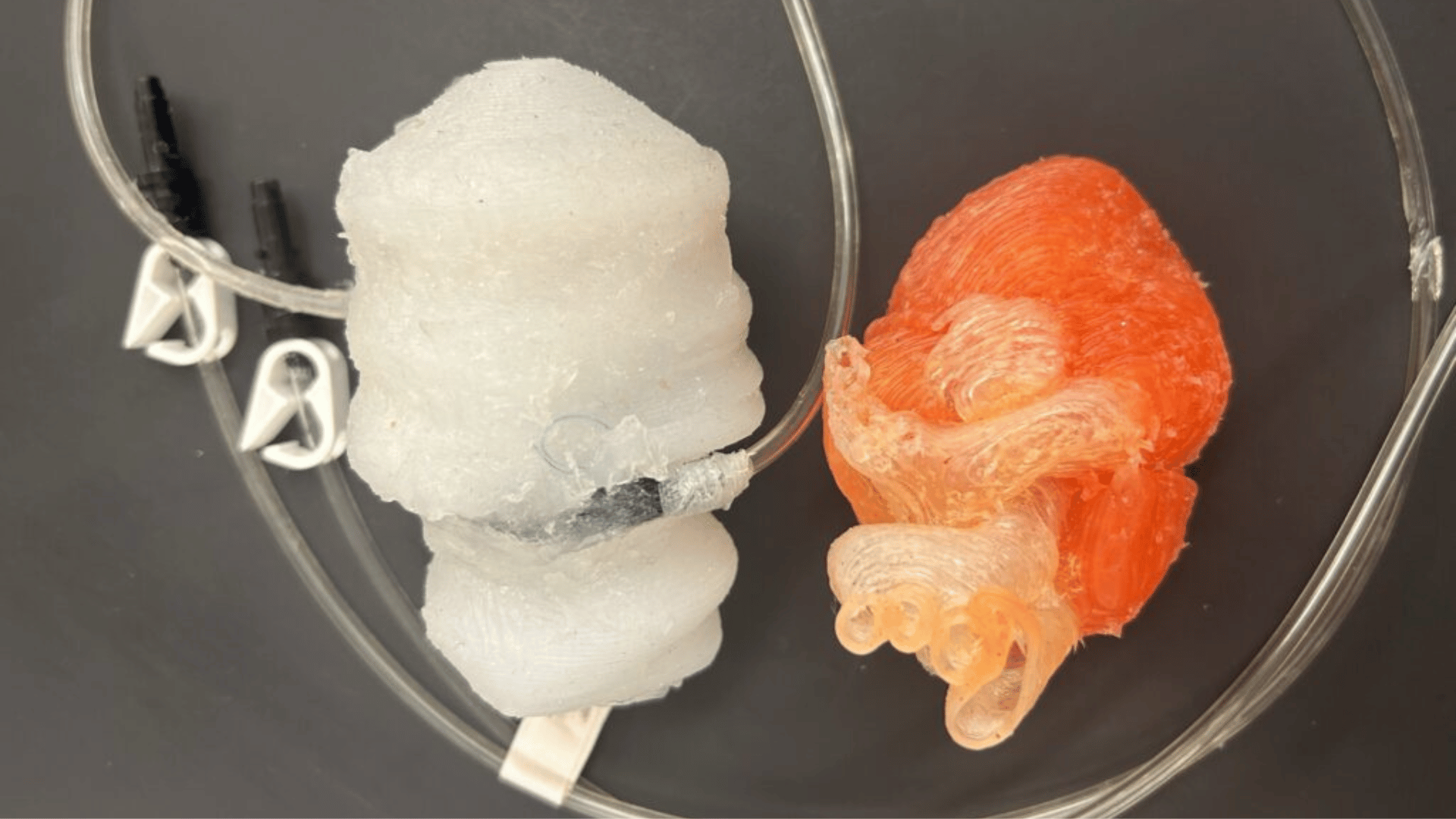
Dr. Ke Huang and his research team developed a biodegradable microneedle patch that delivers a therapeutic molecule directly to injured heart tissue. According to the researchers, it promotes repair and improves long-term function.
Microneedle Patch For a Damaged Heart
The damaged muscle beneath the heart’s outer layer is difficult to access. However, the patch has a unique system that can penetrate it. Each of the patches’ dissolving needles is loaded with the key immune-regulating molecule interleukin-4 (IL-4). “This patch acts like a bridge,” said Dr. Huang. “The microneedles penetrate the outer layer of the heart and allow the drug to reach the damaged muscle underneath, which is normally very hard to access.“
Advertisement
Localized delivery is crucial for therapeutic success, Dr. Huang explained. “Systemic delivery affects the whole body,” he added. “We wanted to target just the heart.“
The core function of this new therapy is to reprogram the body’s inflammatory response. After a heart attack, immune cells, known as macrophages, can exacerbate inflammation and contribute to the formation of harmful scar tissue. Delivering IL-4 directly to the injury causes the cells to shift from a pro-inflammatory state to one that supports healing and scarring reduction.
“Macrophages are the key,” Dr. Huang emphasized. “They can either make inflammation worse or help the heart heal. IL-4 helps turn them into helpers.”
During their study, researchers revealed unexpected benefits. According to the research team, the treatment was observed to enhance communication between heart muscle cells (cardiomyocytes) and the cells lining blood vessels (endothelial cells). “The cardiomyocytes weren’t just surviving, they were interacting with other cells in ways that support recovery,” Dr. Huang explained.
Currently, the treatment requires open-chest surgery. However, Dr. Huang envisions a future minimally invasive design, potentially through a small tube, which would make this concept more practical for clinical use.