A revolutionary stem cell gene therapy, developed by the University of Manchester, is offering a curative possibility for children with the devastating genetic condition Hunter syndrome (MPS II). Three-year-old Oliver (Ollie) Chu became the first patient to receive the treatment. His parents report dramatic progress following the procedure at Royal Manchester Children’s Hospital (RMCH).
Overcoming Limitations of Current Care For Hunter Syndrome


Hunter syndrome is a rare, inherited disorder where a faulty gene prevents the body from producing a vital enzyme needed to break down complex sugar molecules. This buildup leads to severe organ damage, physical decline, and, crucially, cognitive decline resembling childhood dementia. The current standard of care is a costly, lifelong, weekly enzyme replacement therapy (Elaprase). While the treatment reduces physical symptoms, it cannot reverse or halt mental deterioration.
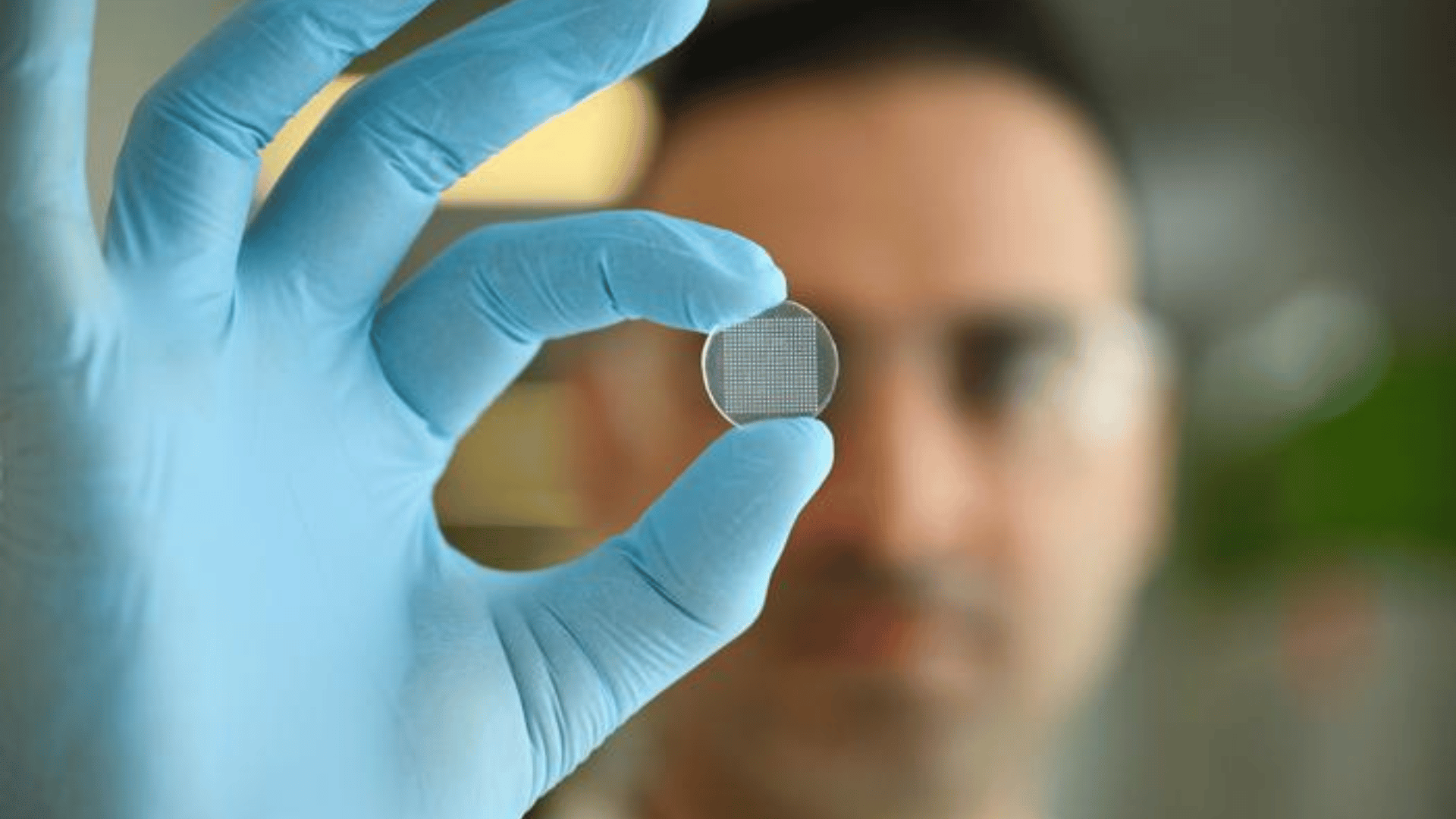
The new therapy, sponsored by the University of Manchester and trialed at RMCH, is a one-off treatment involving genetic modification of the child’s own stem cells. These corrected cells are re-injected, acting as an internal factory to produce the missing enzyme.
Professor Rob Wynn, Consultant Paediatric Haematologist at RMCH and joint clinical lead, said, “Gene therapy is not only safer and more effective, but it enables us to use the child’s own cells which cuts out the need to find a donor, and means we can produce more enzyme for the patient.”
Advertisement
A key innovation, developed over ten years by Professor Brian Bigger at the University of Manchester, is an added tag on the enzyme that allows it to cross the blood-brain barrier. This targets the central nervous system, aiming to prevent the “devastating dementia-like decline.”
Clinical Results
Clinically, Ollie’s results are encouraging. Professor Simon Jones, Consultant in Paediatric Inherited Metabolic Disease and joint study lead, confirmed that Ollie has successfully stopped his weekly Elaprase infusions. Additionally, his blood tests show “very high levels” of the previously missing enzyme, which is an encouraging sign that the treatment is working.
“We’re excited for Ollie’s future, Ollie’s father, Ricky, said. “Seeing the difference for Ollie pre-and post-transplant has made us believers.”
Ollie is the first of five children participating in the study. Researchers are optimistic that the principles underpinning this therapy could eventually be applied to treat many other genetic conditions in addition to Hunter syndrome.